About Sleuth
Sleuth by the numbers*
-
62,000
contributors
-
5,100
new answers daily
-
285
topics covered
-
5,300
app installs/month
-
4/5 app store rating
-
68%
impression-to-install
*as of Dec 2023
What was Sleuth?
Sleuth created a radically different approach for tracking kids’ health and development.
Unlike feedback from annual health check-ups, Sleuth gave parents benchmarks based on the exact day of a child’s age. We filled the gaps in research covering how kids evolve – getting all the leverage we could out of data from 62,000 parents covering 285 topics.
At Sleuth, we focused on common challenges that cause parents to worry but don’t (initially) motivate them to seek experts’ advice: irregular sleep, challenging eating habits, speech development, anxiety, energy levels, tantrums, and so on.
It’s just amazing that you took a pretty hard moment for parents and are turning it into something so useful.
Mother of two in Menlo Park, CA
The Sleuth app had tight feedback loops that drove heavy engagement. Parents using Sleuth instantly saw benchmarks for the general population of U.S. kids for every question they answered.
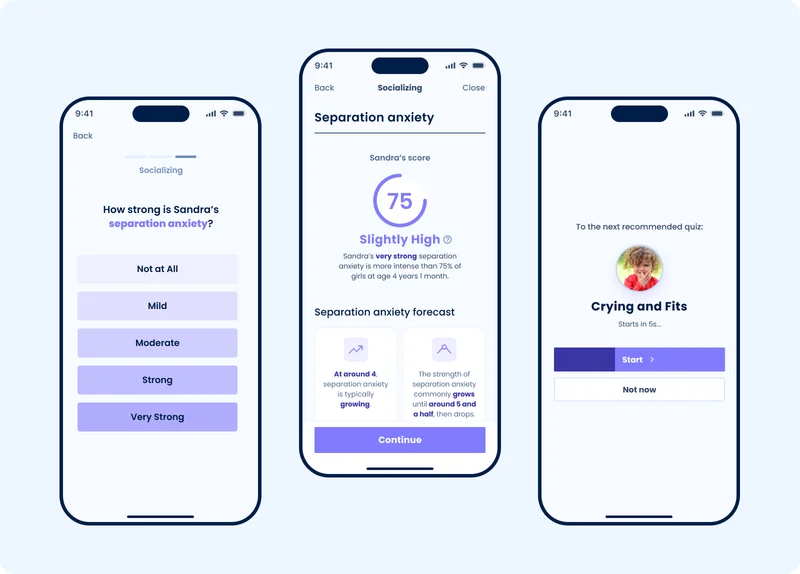
We created consistent methods for measuring any symptom, behavior, and development (severity, strength, frequency, duration). This made for a much easier user experience. Sleuth’s questions were fast and familiar regardless of topic.
Parents sought Sleuth for invaluable data that they could find nowhere else. By joining Sleuth and volunteering to contribute, Sleuth’s data grew by up to 5,000 answers per day.
Why we made it
-
Diagnose early
As many as 50% of critical care interventions are missed by parents, teachers, and doctors at their ideal time.
-
Unresolved questions
In Sleuth’s research, 94% of parents reported a “recent” concern about their kids’ health or development.
-
Continuous healthcare
We treated health as a continuous process flowing from a child’s personal arc, rather than a response to incidents.
-
Local information
Children’s caretakers are the unique go-betweens for doctors, schools, therapists, and children’s programs. They alone provide day-to-day child care.
-
Natural language
Sleuth captured everyday & longitudinal observations in parents’ own words. This was essential to build an AI that communicated from their perspective.
-
AI in pratice
Sleuth put machine learning and AI at the center of our designs. Our internal tests had strong diagnostic accuracy based on parents’ unstructured, everyday words.
-
Diagnose
earlyAs many as 50% of critical care interventions are missed by parents, teachers, and doctors at their ideal time.
-
Unresolved questions
In Sleuth’s research, 94% of parents reported a “recent” concern about their kids’ health or development.
-
Continuous healthcare
We treated health as a continuous process flowing from a child’s personal arc, rather than a response to incidents.
-
Local information
Children’s caretakers are the unique go-betweens for doctors, schools, therapists, and children’s programs. They alone provide day-to-day child care.
-
Natural language
Sleuth captured everyday & longitudinal observations in parents’ own words. This was essential to build an AI that communicated from their perspective.
-
AI in pratice
Sleuth put machine learning and AI at the center of our designs. Our internal tests had strong diagnostic accuracy based on parents’ unstructured, everyday words.
Two product stages
Sleuth v1: Starting with storytelling
We built Sleuth v1 to support long-form storytelling by parents – as well as timelines of symptoms, diagnosis, treatments and outcomes.
Stories created a sense of community – and included essential detail. We discovered that stories frequently had important practical advice about how parents could approach doctors for their concerns and exactly whom to seek out.
In Sleuth V1, we also offered developmental and behavioral assessments. We reached out to leaders in pediatric research to get free access to authoritative, evidence-backed sleep, development, eating, and behavioral questionnaires.
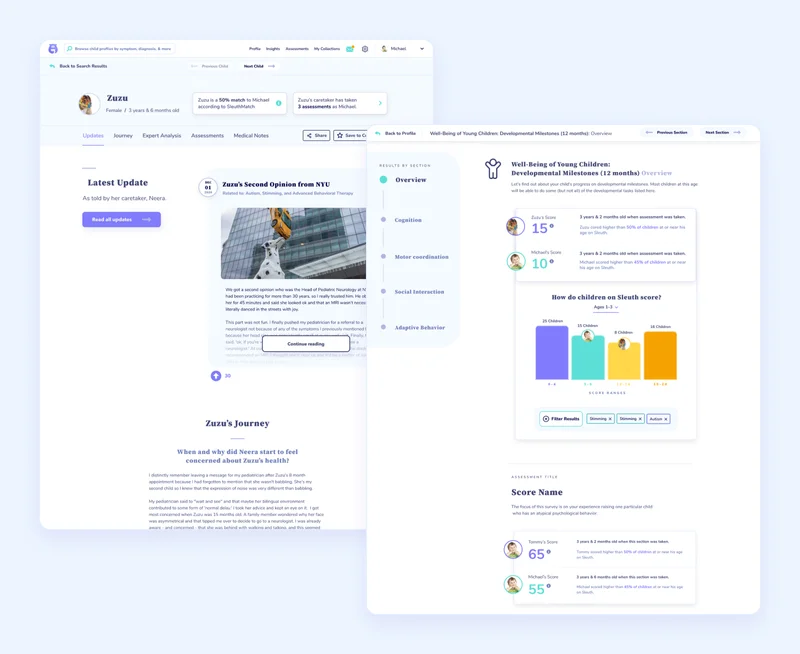
More than 90% of people who visited Sleuth’s website either clicked on profiles or completed assessments.
Sleuth v1 was built with funding provided by Antler.co and Newlab.com in partnership with Ridgebox.com.
Sleuth v2
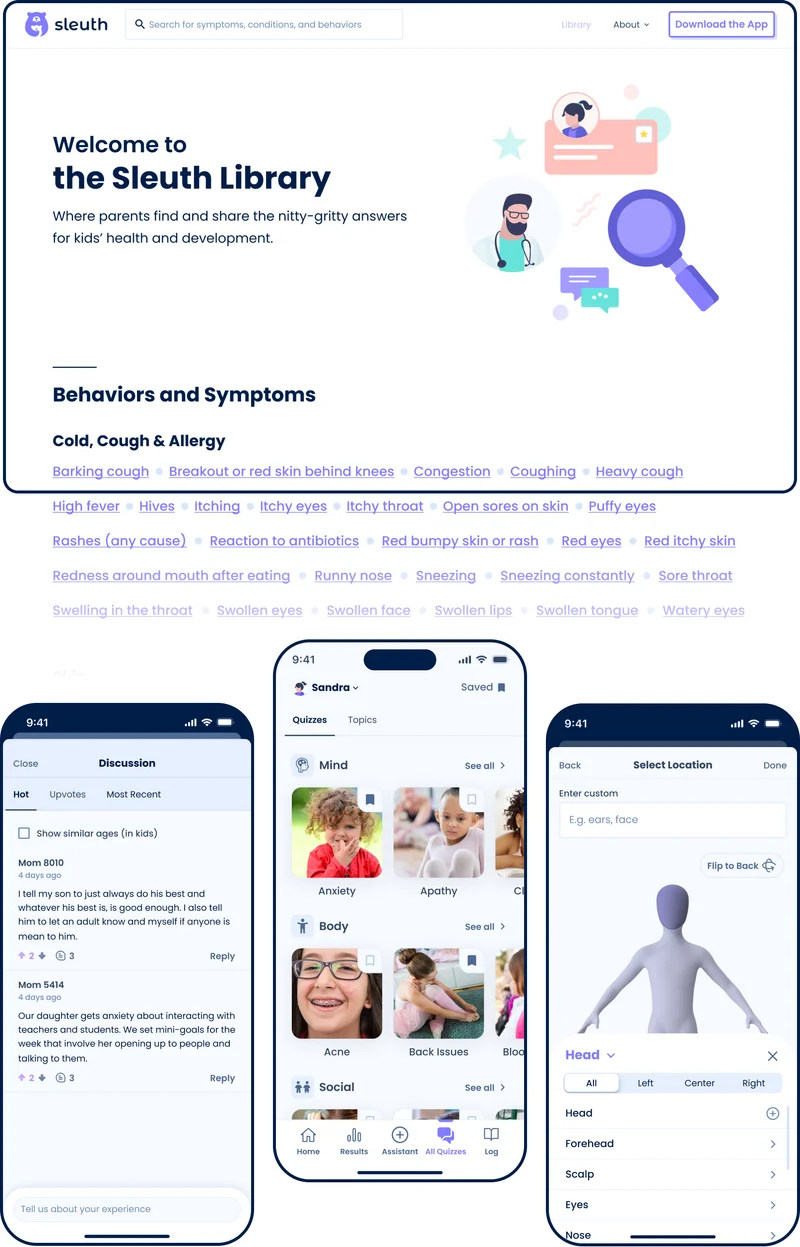
Sleuth v2 reflected parents’ demand for more quizzes and more quantitative feedback.
We used classic qualitative coding and ML-based clustering with OpenAI’s text-embeddings to surface 250 foundational topics in 30,000 child health histories.

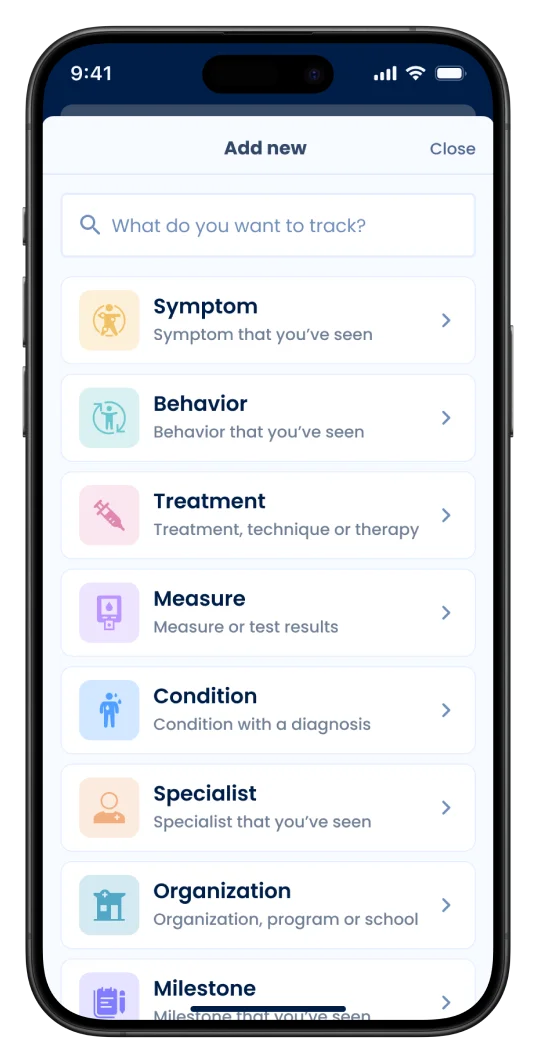
Version 2 included:
- Assessments: 70+ original, extensively validated short quizzes covering 285 topics
- Logging/Tracking: Tools for tracking events related to any symptom, behavior, treatment, program, or specialist. Parents could upload files/video and take notes.
- Library of symptoms, conditions, and treatment data: A library of data and and summary statistics built from our existing content.
- Discussions: Tools to allow parents to discuss any topics in the extensive library.
Sleuth v2 was built with funding provided by Brooklyn Bridge Ventures, Math Venture Partners, Graham & Walker, John Friedman, Gary Vaynerchuk, and other outstanding angel investors.
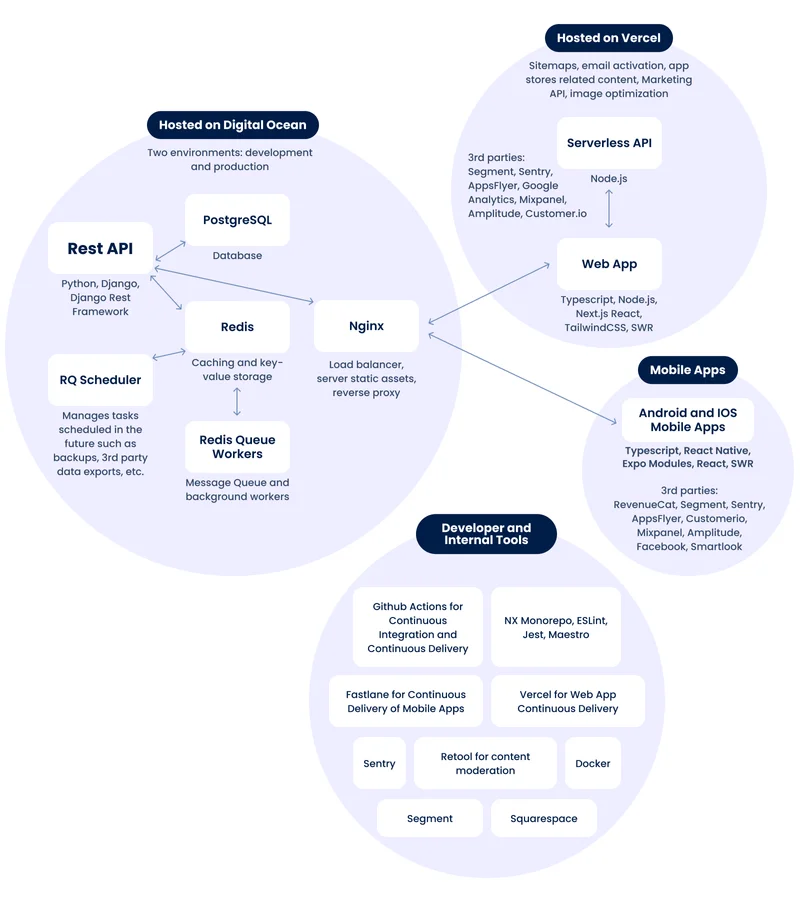
Tech Infrastructure
We built Sleuth with several considerations:
- established architecture and frameworks;
- ability to quickly scale horizontally for millions of users if necessary, without over-engineering in the meantime;
- flexibility to move data/cloud, switch out tools and architecture;
- prioritizing quality and development speed.
We kept a healthy balance of essential testing and continuous delivery for a small team. At the same time, there were numerous technical improvements we shelved for a later date.
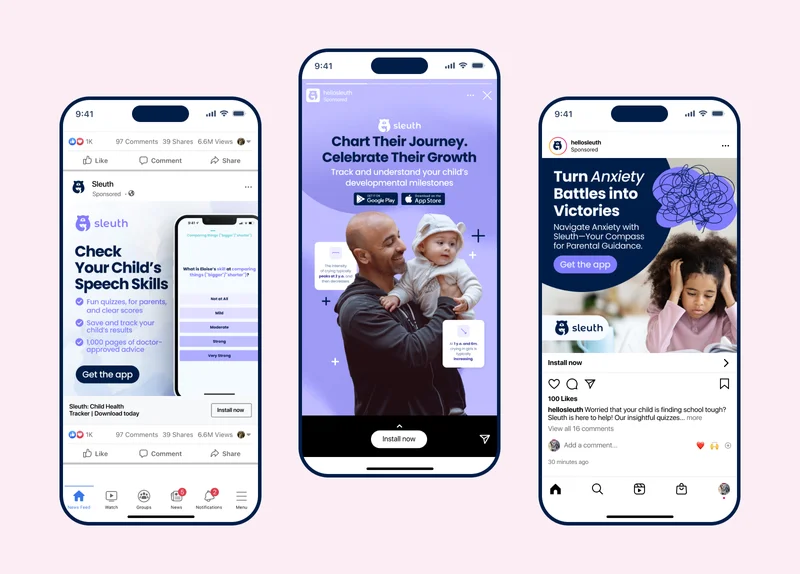
Marketing
Sleuth ran an efficient marketing engine working closely with a UK-based agency called Favoured. We noticed that few healthcare organizations use social media ads to target specific health symptoms and developmental concerns, even though many of these affect 5% to 20% of all children at some point in their lives. This created an opening for exceptionally efficient marketing that scaled horizontally across thousands of specialized keywords from “tantrums” to “motor skills”.
Activity on Sleuth
Sleuth’s growth took off in the 3rd quarter of 2023. Our parent community answered 28,000 questions per week in the app, beating our goals of pacing at 1 million answers per year before the end of 2023.
![A line graph titled 'Quiz Topic Completed [Total Events]' showing a sharp increase in events for the Sleuth app. The timeline starts on September 18 and ends on December 3, 2023. Initially, the line is flat, indicating stable event counts. However, there is a steep climb starting in November, peaking at 28,262 events in the last recorded week, which is a 23.75% increase from the previous week. The chart highlights significant growth in user engagement with the quizzes.](/_astro/chart1.C7lVKU0f_Z2s3cMz.webp)
Sleuth organized its 70+ quizzes into different themes, and about 60% of people get very into those quizzes – quickly completing 5 or more.
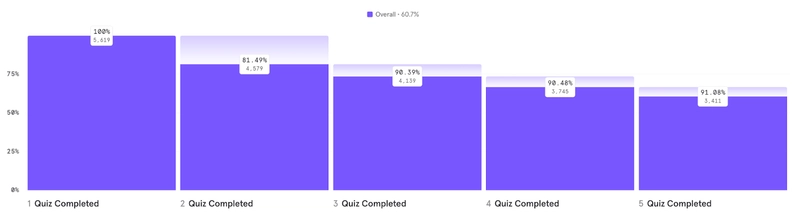
We routinely saw individuals who answered hundreds of questions per day.
Here were some of the biggest Sleuth community topics:
- Crying, fits, and tantrums (especially in young kids)
- ADHD-related worries: restlessness, difficulty sitting still, difficulty paying attention
- Child anxiety-related concerns: separation anxiety, constant worry
- School-related concerns: anxiety about school, difficulty focusing on homework, etc.
In the media
Sleuth received favorable coverage in:












Who we were
Core team
-

Alex Leeds
Co-Founder & CEO
-

Sehreen Noor Ali
Co-Founder & President
-

Georgiy Tarasov
Founding Engineer
-

Alyona Korysta
Design Leadership
Partners
-

Alexander Polekha
Software Engineer
-

Igor Veselov
Software Engineer
-

Jade Glaze
Engineering Manager
-

Jenna Cunningham
Digital Art
-

Regina Dacio
Social Media
-

Sam Battles
Performance Marketing (Favoured)
Advisers
-

Camille Proctor
Condition Strategy
-

Chethan Sarabu
Pediatrics & Product
-

John Friedman
Strategy & Finance
-

Shaun Hinklein
Growth Marketing
Really, it has been other parents that have helped me to figure out this world. They have suggested treatments. They have told me things I should ask doctors about when I didn't know as much. And now… I find myself answering questions for others.
Donia, Mother in of two in FL

